What is the HORIZON-HLTH-2026-01-DISEASE-03 Horizon Europe call?
Prevention, diagnosis, and treatment of post-infection long-term conditions
Opening
10 February 2026
Deadline
Keywords
Cluster health
post-infection long-term conditions
RIA
disease Prevention
disease pathogenesis
clinical decision-making
targeted interventions
Your microfluidic SME partner for Horizon Europe
We take care of microfluidic engineering, work on valorization and optimize the proposal with you
HORIZON-HLTH-2026-01-DISEASE-03
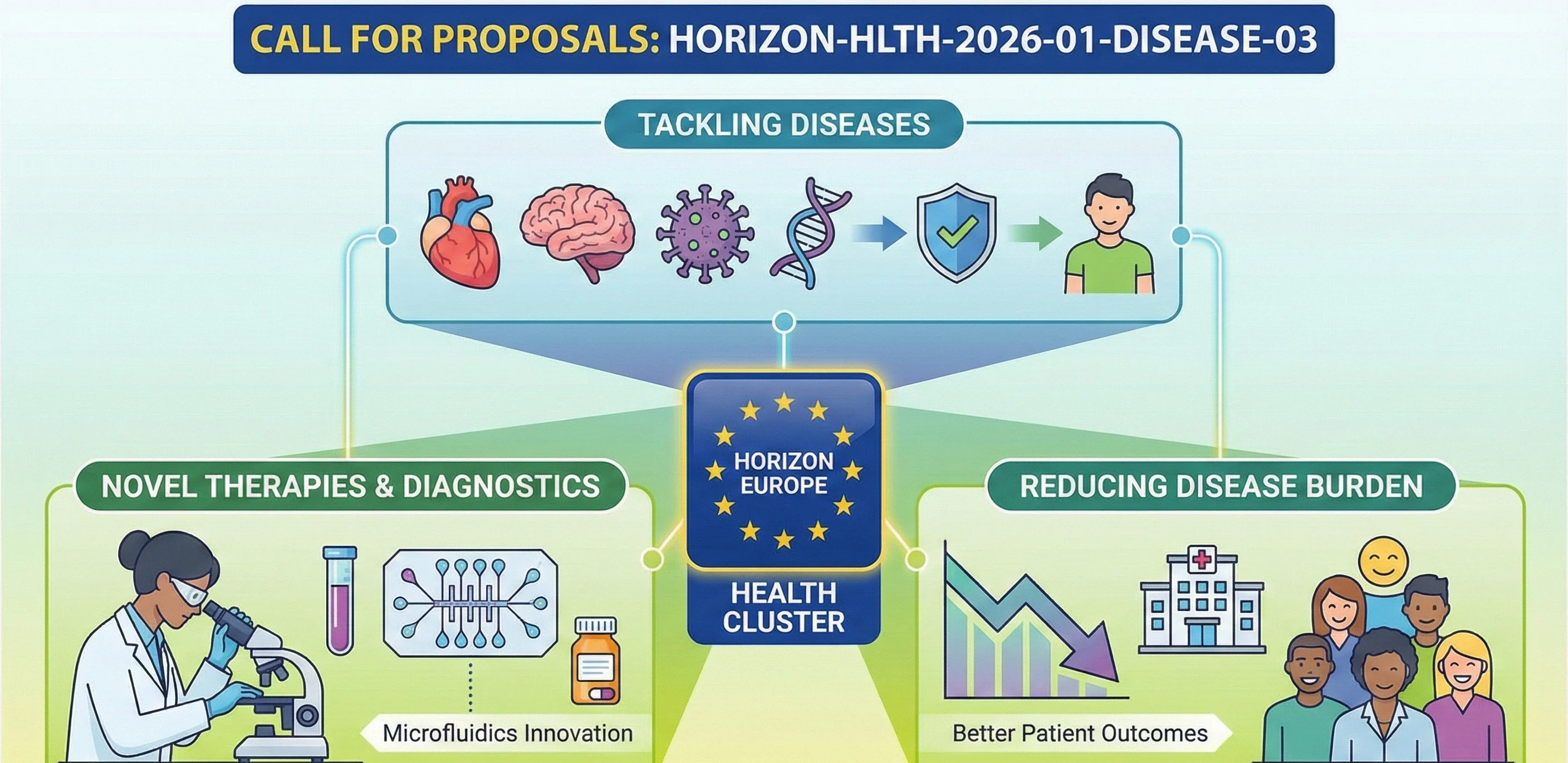
It is a topic for funding Research and Innovation Actions (RIA) in Horizon Europe Cluster 1 – Health (Single stage – 2026) to promote the prevention, diagnosis, and treatment of post-infection long-term conditions.
Discover more!
Administrative facts: what do we know about the HORIZON-HLTH-2026-01-DISEASE-03 call?
Which call is it under?
- Name of the call: Call – Cluster 1 – Health (Single stage – 2026)
- Call number: HORIZON-HLTH-2026-01.
- Destination: Tackling disease and reducing disease burden
What is the opening date and the deadline?
- Opening date: 10 February 2026
- Deadline: 16 April 2026
- Deadline time: 17.00 Brussels local time
What about the budget and estimated size of the project?
- The subject of the topic: The development of research on the prevention, diagnosis, and treatment of post-infection long-term conditions.
- Type of action: RIA
- Overall topic budget: EUR 39.30M.
- EU contribution expected for individual projects: EUR 6.00-8.00 million.
- Nominal number of funded projects: 5.
Deadlines of European Programmes
Download the MIC Horizon Europe 2026/2027 Calls Calendar:
-All Horizon Europe deadlines (by cluster and call).

Scientific range: what the Commission expects from the HORIZON-HLTH-2026-01-DISEASE-03 grant
What outcomes are expected?
The outcomes anticipated of projects are expected to encompass:
- Improved knowledge of the pathophysiology and disease pathogenesis, including the predictors of risk and targets of therapy of long-term conditions after infection.
- Favor the identification of new diagnostics (such as biomarkers), therapy-relevant targets.
- Better knowledge of the disease process, its subtypes, and the possibility of determining populations at risk.
- Evidence that leads to improved prevention and management, to the enhancement of the quality of life, and to the reduced load on patients and healthcare systems.
What is within scope?
- The subject is aimed at long-term disorders caused by any type of microorganism (including viruses, bacteria, parasites, and fungi) that persists after the primary infection has resolved.
- The burden includes delayed recovery, ongoing damage, and possibly worsening of pre-existing disease, as well as heterogeneous symptoms across multiple organs and systems.
What are the specifically proposed research directions?
Research lines which are pointed out in the Work Programme include:
- Prevention and treatment, such as biomarker identification, the development of new diagnostic methods, and the creation of targeted interventions.
- Mechanisms and risk factors (e.g., host factors (e.g., genetic/epigenetic, immune response, viral persistence, microbiome dysbiosis), pathogen/organ interaction, and so on).
- Multi-omics / systems: Identify pathways and targets (e.g., proteomics, metabolomics, epigenomics, transcriptomics).
- Greater disease trajectory and subtype characterisation between patients and conditions.
Scientific strategy: How can you enhance your chances of being funded through HORIZON-HLTH-2026-01-DISEASE-03?
- Make your project high-impact
The higher the burden on society, the higher the chances of being funded. This can be a pathogen that impacts a high number of people, or where the long-term consequences of infection are especially severe. Reducing the disease burden on society and the healthcare system is important.
- Base all on the four deliverables of the evaluator.
Mechanism: This is the process by which a clinical or scientific intervention causes or prevents disease. Risk factors/subgroups: This is the information about risk factors in an actual case that may lead to disease or prevent it. Biomarkers/diagnostics: This is where the clinical/scientific process takes place in an actual disease case to facilitate or avert disease. Actionable prevention/management evidence: This is where clinical/scientific processes occur in real disease settings to enable or prevent disease. When one is not present, you are off course with what is expected.
- Take subtypes as an objective of central scientific activity, rather than an addition.
Clinically and biologically, clearly plan to stratify and demonstrate the impacts of stratification on prevention/diagnosis/management pathways.
- Be very specific regarding biomarkers.
Not: we will discover biomarkers, but: What are the types of specimens, at what times, or by what methods shall we analyse them, by what logic our analysis will be validated, and how their analytical value will be translated into clinical action (or clinical decision-making): into triage, into monitoring, into the choice of therapies.
- Demonstrate how to relate multi-omics to decision-making.
The subject names multi-omics approaches; the evaluators will seek to find a line of thinking starting with omics signals – pathways – targets – diagnostics/management evidence.
Consortium & proposal-writing plan: what works best with this type of Health RIA?
- Develop a triangle of bench – bedside – health system.
-Mechanisms & biology (immunology, infection biology, systems biology)
-Clinical phenotyping & cohorts (hospitals, primary care, long follow-up capacity)
-Implementation relevance (public health/health economic / guideline or pathway expertise)
- Be clear concerning patient relevance.
The anticipated results cover both quality of life and the burden of healthcare; this is plausible when a patient organisation structures patient involvement.
- Write in results-first writing style.
Evaluators skim. Put the “so what?” early: what new diagnostic competence, what subgroup identification, what evidence on prevention/management, then how do you get there.
- Low profile yet productive step: involve a new SME.
Practically, SMEs enhance the credibility of diagnostics, data tooling, biomanufacturing/assay industrialisation, and exploitation directions (without turning the proposal into a product pitch).
How would microfluidics contribute to this topic?
Microfluidics may conveniently be a boost juice to the very “biomarkers + mechanisms + stratification” backbone of the call:
- Sensitive biomarker assays- microfluidic sample preparation + multiplexed lower abundance inflammatory/metabolic assays (improved signal with low volumes).
- Single cell immune profiling: microfluidic droplets and chips to map immune states associated with persistent symptoms and risk groups.
- Organ-on-chip / infection-on-chip models: The microphysiological systems can be used to investigate persistence, immune dysregulation, vascular engagement, microbiome-host interactions, and are useful in mechanism-to-target logic.
- Point-of-care / decentralised testing: your project needs to be in the real-world of diagnosis or monitoring, microfluidics can enable you to develop prototypes in less time.
The MIC already brings its expertise in microfluidics to Horizon Europe:
H2020-NMBP-TR-IND-2020

Microfluidic platform to study the interaction of cancer cells with lymphatic tissue
H2020-LC-GD-2020-3

Toxicology assessment of pharmaceutical products on a placenta-on-chip model
FAQ - HORIZON-HLTH-2026-01-DISEASE-03
So what is it that this call is all about?
The target audience of this call is the population that overcomes infections yet is not fully recovered- persistent fatigue, dysfunctional organs, cognitive difficulties, immune dysregulation that persists months or years after the pathogen has been eliminated. It is not only the ability to describe such conditions but also the opportunity to understand the mechanisms, define who is vulnerable, create diagnostics, which are applicable in medical practice, and develop interventions that can better the outcomes. Consider post-viral syndromes, chronic complications of bacteria. It is regarding the conversion of descriptive medicine into actionable medicine in long-term conditions, in the post-infection period.
Who is supposed to apply and how much money is available?
The most powerful consortia are three-world bridges: bench scientists with the ability to dissect mechanisms (immunologists, systems biologists), clinical teams with patient cohorts and the ability to follow them longitudinally, and implementation experts (health economists, guideline developers). Patient organizations should be included from the beginning. EUR6-8 million is allocated to individual projects (36-48 months) on average. A EUR39.3 million envelope is going to fund approximately five projects. Deadline is April 16, 2026. They are Research and Innovation Actions that are aimed at creation of knowledge that has clear implementation routes.
What are the infections that are in scope?
Intentional wide – any microorganism that causes persistent conditions despite resolution of acute phase. Viruses, bacteria, parasites, fungi. Pathogens with an estimated high impact on society and the healthcare system will be of importance.
Which four outcomes are the evaluators really seeking?
To begin with, better knowledge of pathophysiology and mechanisms, including proven risk factors and treatment sites. Second, new diagnostic features -biomarkers that are reliably measured, assays that are effective in the clinical environment, decision-making stratification tools. Third, the enhanced characterization of the disease with clinically meaningful subtypes and the means of identifying population at risk. Fourth, results leading to better prevention and management guidelines, proving to cut down patient load and burden on the healthcare. When you are a great mechanism person with a poor clinical translation, or the reverse, you are not competitive. Address all four credibly.
In what way ought we to arrange the scientific work intelligently?
-Stratification is not an add-on; it should become a key goal. Clearly define how to delineate subtypes based on biological processes or clinical development and progression, and demonstrate the impact of stratification on the pathway of care.
-Be precise regarding biomarkers, not: we will determine markers, but rather: the specifics of the specimens you will collect, and when and with which platforms you will accomplish this, on a validated outcome against what decision.
-Demonstrate an effectively clear line: multi-omics data – biological pathways – actionable targets – diagnostic or therapeutic prototypes.
-Write results-first, lead with so what (new diagnostic capability, subgroup identification, prevention evidence), and then write the methodology. Skimmer evaluators bring out the logic at the outset.
What is the microfluidics value-added in this case?
There are four contributions in concrete.
To begin with, sensitive biomarkers assays -microfluidic sample preparation and multiplexed detection of low-abundance inflammatory or metabolic biomarkers using small volumes, essential in longitudinal patient sampling.
Second, droplet or chip-based immunophenotyping of a single cell type profiles the dynamics of cells related to enduring symptoms and sorts high-risk populations at impossible-with-bulk-methods scale.
Third, organ-on-chip and infection-on-chip models offer controlled microphysiologic systems studies of persistence, immune dysregulation, vascular involvement, host-microbiome interactions, connecting mechanism to target.
Fourth, point-of-care prototyping allows the creation of decentralized diagnostics that can be used at the primary care or at a remote location. This deals with the backbone of the biomarker-mechanism-stratification of calls.
What is the true competition of a consortium?
-Relevance to patients should be clear and integrated, and convincing when patient organizations collaborate to design participation from design through dissemination.
-Addition of specialized SMEs to enhance the development of diagnostics, data analytics platform, industrialization of assays, or pathways to exploitation-relevant and not pitched by the product.
-Show how work will have an impact on clinical guidelines or healthcare pathways, and not undefined translation assurances.
-Demonstrate the entire bench-to-bedside arc with mechanisms that guide clinical work and clinical observations to be the impetus behind mechanistic questions.
-Risk management of project-specific scientific and implementation issues, and not boilerplate.
-Roadmap with timeline gates enabling you to kill deadlines and bet on successes.
What is strictly in and out of scope?
-In scope: long-term diseases of any microorganism (viruses, bacteria, parasites, fungi) that remains after disease that initially occurred is removed. The costs are that of delayed recovery, continued damage, aggravation of existing disease, heterogeneous symptoms that involve more than one organ system.
-The areas of research are biomarkers, developing diagnostic methods, targeted interventions, host (genetic, epigenetic, immune response, viral persistence, microbiome dysbiosis) factors, pathogen-host interactions, multi-omics pathway discovery, disease progression and subtype features.
-Out of scope theoretical work that has not yet been validated, proposals that lack the implementation courses to healthcare systems.
What are the pitfalls that usually destroy Health RIA proposals?
-The discovery of biomarkers without severe validation, performance of analysis or plan to use it in clinical applications.
-Stunning multi-omics and no description of the way results are used to make decisions. Lacking or only generally formulated risk management instead of problem-solving project-related challenges.
-Consortia lacking implementation knowledge, or clinical and mechanistic depth.
-Performative, not integrated, patient involvement.
-Losing the health economics logic or guideline pathway logic, which relates research to real-life healthcare change.
-Buzzy words without actual goals and realistic steps of improvement.
What do timelines and milestones show in terms of credibility?
Plan work packages based on the four categories of outcomes (mechanisms, risk stratification, diagnostics, management evidence) instead of the customary disciplines. Apply decision gates where the management process is flexible- cancel weak and reinforce winners. The initial milestones define reproducible practices and test major assumptions. Mid-term measures involve the diagnostics of prototypes or interventions in the pertinent populations. The late-stage milestones provide evidence packages that can be used by the guideline developers or by regulators. Present quarterly review points wherein consortium will indicate whether a particular scientific line is progressing as per the criteria. The alignment of the budget to concrete milestones in risk reduction can be easily read, that you know how to produce interesting data as opposed to producing implementable knowledge altering clinical practice.
