A microfluidic system for oocyte maturation and in vitro fertilization: EUROVA
Author
Christa Ivanova, PhD
Publication Date
September 14, 2021
Status
Keywords
oocyte maturation
in-vitro fertilization
in-vitro maturation
oocyte culture
clinical embryology
fertilization success
Hormonal cues
Your microfluidic SME partner for Horizon Europe
We take care of microfluidic engineering, work on valorization and optimize the proposal with you
A microfluidic system for oocyte maturation and in vitro fertilization: introduction
An oocyte is a female germ cell involved in the process of reproduction. In the natural environment, the oocyte in young females before puberty is arrested at the first meiotic division as the primary oocyte within the ovary.
After reaching puberty, the luteinizing hormone (LH) surge leads to the resumption of the arrested meiotic division, and the pituitary gonadotropin stimulates the completion of the first stage of oocyte maturation right before ovulation. The oocyte is contained in this state till it is the time for fertilization. The second meiotic division starts during fertilization, and the second stage of oocyte maturation is completed.
Here, we describe novel approaches to studying oocyte maturation and in vitro fertilization with the help of microfluidics.
Improving in vitro fertilization with microfluidics: project description
During in-vitro fertilization (IVF), the fertilization process of fusion of male and female gametes is carried out externally before inserting the mature oocyte into the female body in cases where male gametes fail to fuse with oocytes naturally. In many cases, it is found that the females are producing only primary oocytes that have not entered the first stage of the oocyte maturation process due to various reasons like chemotherapy, advanced age, etc., which hampers IVF procedures.
This is where in-vitro maturation (IVM) comes into the picture, where the primary oocyte is collected, and the maturation process is carried out externally in the lab. The rate of successfully maturing the oocytes externally depends on the age of the female from whom it is collected, the quality of the primary oocytes collected, and the in-vitro conditions.
Microfluidics can help advance the in vitro fertilization field by recreating a physiologically relevant environment and allowing precise control of conditions.
An accurate natural oocyte environment for extended periods during the study is required to conduct a deeper study of oocyte maturation and thus improve the efficiency rates of in vitro maturation and fertilization processes.
Microfluidics is a perfect fit for studying oocyte maturation as it gives the user exact control over the oocyte culture environment by controlling the microfluidic channel environment.
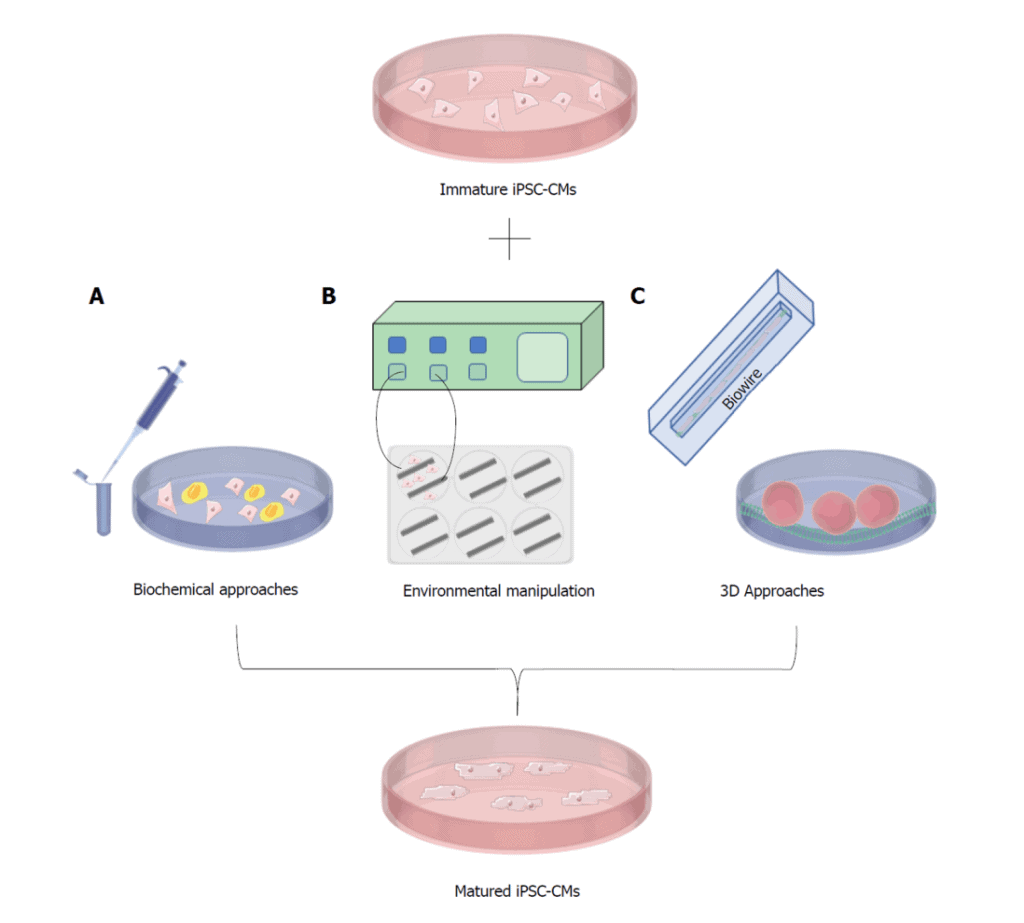
Image source: Machiraju, P. and Greenway, S., 2019. Current methods for the maturation of induced pluripotent stem cell-derived cardiomyocytes. World Journal of Stem Cells, 11(1), pp.33-43.
This project has received funding from the European Union’s Horizon 2020 Marie Sklodowska-Curie Innovative Training Networks program under grant agreement No 860960 (EUROVA).
Researcher

Aaditya Venkatesha Babu Bangaru
Marie-Curie PhD candidate Elvesys/University of Ghent
- M.Sc. in Nanotechnology (Chalmers University of Technology, Sweden)
- B.Eng. in Mechanical Engineering (Visvesvaraya Technological University, India)
Areas of expertise:
Surface acoustic wave sensors, microfluidics, 3D Modeling, Nanotech, Conducting Polymers, CNC.


Check our Projects
FAQ – Oocyte maturation and in vitro fertilization: EUROVA
What is the EUROVA project?
EUROVA investigated the possibility of networking the micro-environment of the ovary and the fallopian tube to achieve oocyte maturation (IVM) and in-vitro fertilization (IVF) using microfluidics. The essence of it is practical: shear, gradients, flow control, and timings have to be adequately managed, which means that delicate gametes must act as they do in the body – only it is on a chip. It was a project funded in the Marie Sklodowska-Curie Innovative Training Networks (H2O2, grant 860960).
What is the rationale of introducing microfluidics in IVM/IVF procedures?
Simple is that of the static wells which have the problem of fine control.
In microchannels you can:
• maintain nutrients and hormones in a fresh state by means of mild perfusion,
• impose both very low, constant shear (usually less than 1 Pa when in contact with oocytes),
• form gradients (hormones, chemokines) in a non-diffusive manner,
• log and automate every step.
The potential implications of this in practice are more reproducible conditions of maturation and fertilization with reduced wastage of reagents.
Which biological processes are current biologically modeled on-chip?
Two important transitions; (i) restoration of the process of meiosis up to metaphase II (oocyte maturation), and (ii) co-incubation between gametes to be fertilized. The platform will not substitute clinical embryology in its entirety; rather it concentrates on the micro-environs which exert the greatest impact on competency and successful early fertilization.
Does the chip prevent the harmful mechanical stress of the oocytes?
Channels and traps have been designed so that they do not narrow down, the flow is operated in the nL–µL/min regime to keep the wall shear small and dead-zone corners are removed to prevent local stagnation. As implemented, or directly calculated, we do seek laminar and predictable profiles as well as the residence times comparable to every culture phase. The outcome is less harsh and far more consistent than the process of pipetting in open wells.
Controllability of inputs (media and signals)?
Hormonal signals (e.g. LH-type stimulates), small molecule agonists, oxygen gradients through gas-permeable substrates, and temperature (usually 37 °C in ±0.1 °C). The timing at which the media is switched can be altered i.e. minutes to hours by flow programs such that tends to resemble more closely the pulsed form of the in vivo signal than the single cocktail.
In what ways does this assist most as compared to the traditional IVM?
Two positions (i) difficult cohorts, e.g. oocytes in the older population or post-chemo, where tight control and handling sensitivity can be important; (ii) development of a protocol, where you are setting protocol parameters and readout and chips allow you to run large numbers of slightly different conditions simultaneously.
How does success in this regard look like?
In the case of maturation step: more oocytes that reach MII with oocyte morphology undistorted and spindle. This is normal in terms of fertilization: a normal pronucleus is formed; there is no abnormal cleavage. Since different labs use different baselines, instead of using a standard percentage we put stress on delta-metrics (better than your existing protocol and with the same readouts).
Can this be co-existent with standard equipment of embryology and a QC?
Yes. Its design is such that it will be placed next to the incubators and microscopes that are already in the laboratory. Start of maturation (PN formation), early cleavage are equivalent to conventional QC. The volumes in the media are minimal and the formulations and sterility limits are similar to the existing SOPs, and this facilitates the validation process.
The structure of EUROVA and who did what?
It was an MSCA network that associated both academic and industrial partners to jointly train researchers, and jointly develop the microfluidic toolkit. MIC performed microfluidic engineering, rapid prototyping, and automation in the consortium – linking the demands of biology and builds manufactured in chip designs.
Will it be able to fit to my biological model or unusual limitations?
That’s our day job. We optimally program channel geometries, surface coats, perfusion programs, and sensor integrations (flow, temperature, occasionally dissolved oxygen) to an assay. To our partners, we transition between CAD into functional prototypes in a very brief time and repeat the process of reading your biology with your chip before adapting the chip to match you instead of the other order.
What should be considered as next steps of a lab/consortium?
Begin with a brief design spurt: stipulate your readouts, tolerable shear/flow margins and design regimen of the media. We would then use that to make a first-pass chip, and a script to automate, a pilot scale run with your existing IVM / IVF process to do the benchmarking and (assuming the data is consistent) embed it in a Horizon Europe or MSCA Doctoral Network package.